A lot of the text used in this section are taken directly from a report produced by Julie Allen and Sharon Sheldrake, who have kindly agreed that we can share it with you.
Why was the project required?
Julie and Sharon noticed that dementia patients were eating sparingly on the hospital wards. After thinking this over, they found that none of the hospital staff are trained in how to support a person to eat. Patients were often sat with food in front of them not being touched. Fluid intake also posed an issue as this is no longe recorded (unless there is a noted medical requirement for this. Preparations for mealtimes were lacking as well (such as, washing hands, clearing tables), leaving the patient wondering when mealtimes actually were. Furthermore, they also found that mealtimes were not considered as an enjoyable experience for patients or the staff members involved, but instead were viewed as a mundane necessity.
Background of the project
Julie and Sharon observed a lunchtime dining experience within the hospital setting, along with Matthew Rowland, Head of Learning and Development from Training 2 Care, with the aim of discovering whether it might be possible to adapt the training that Training 2 Care provide called D.I.E.T (Dining Immersive Experiential Training), specifically for the hospital setting.
There were a series of key points noted at this time:
- Lack of preparation before food was bought out to the patients (such as hand washing, taking people to the toilet, moving items off of their tables)
- Background noises, which may be a distraction to patients (such as telephones ringing, people coughing, rubbish bags being rustled, squeaking doors, staff members talking, equipment trollies wheeling around the ward)
- The food menus were text focused and had limited use of images
- Some staff members were wearing face masks during mealtimes, despite it not being required, which appeared to cause some difficulty for the patients in hearing and understanding clearly
- Meals being served on the overbed or chair tables, despite these often already having a variety of objects on them already, making the tables increasingly cramped
- It appeared as though there was a lack of acknowledgement of how the patient was positioned for their meal (such as, if they were sitting upright, in a comfortable position to eat, for example, one patient looked as if they were hunched over the table while attempting to eat
- Some of the meals were placed out of reach of the patient
- Some of the patients required assistance to eat and were not communicated with about the support they wished to receive. It appeared as though the staff observed were feeding these particular patients using the direct hand technique as default, some of which were wearing face masks, further enhancing the communication barrier for the patient
- Frequently staff members were standing over the patients that required assistance eating, rather than sitting alongside the patient and interacting with them
- Majority of patients received minimal interaction from staff members during the observed mealtime
- A patient was witnessed who was struggling to pour a drink for herself and then proceeded to ask for assistance. The patient was attended to, however the staff member did not discuss her requirement, they simply poured the drink for her. It would have been more beneficial for the patient to promote their independence and offer support through the hand over hand method, for example.
- Patients had restricted mealtimes, we witnessed the plates being collected after approximately 15-20 minutes, regardless of whether the patient had finished their meal, or even if they had started it
As a result of the observation, three key factors were noted that had to be addressed to adapt the D.I.E.T training specifically for the hospital setting:
- Communication and interaction with patients during mealtimes; and
- Finding methods for staff to use that provide support to patients, whilst encouraging patient independence
- Preparation letting patients know that mealtime is soon, clearing bedspace, hand washing, toileting.
Methodology
Following the observation, it was agreed that a D.I.E.T showcase would be held for professionals within the hospital where attendees would be given a taster version of the course. The showcase was well received by all attendees and staff members from a vast scope of the medical profession arrived; including a speech and language specialist, occupational therapists, consultants, doctors, the assistant director of nursing, mouthcare, the quality improvement lead, dieticians, and housekeepers. Those that attended provided Julie and Sharon with valuable feedback for them to further develop the D.I.E.T training for the hospital setting. This was followed by a review of original Training 2 Care course content to determine what adaptions would need to be made to the course to make it suitable for the hospital setting.
A series of changes were made to the course by Matthew Rowland, based on feedback provided by Julie and Sharon, making the course tailored specifically to hospital settings. This included amending both some of the content covered, and how the course was to be delivered.
A closed questionnaire was created to be given to staff members, patients and housekeepers, to be completed before and after training had been given. Following this, a Plan Do Study Act chart was created and a Quality Improvement Project was begun.
It was agreed that a D.I.E.T training programme would be conducted for the hospital setting which would be given to two wards. When choosing the wards to use for the trial, the choice of wards was limited to those primarily caring for the elderly.
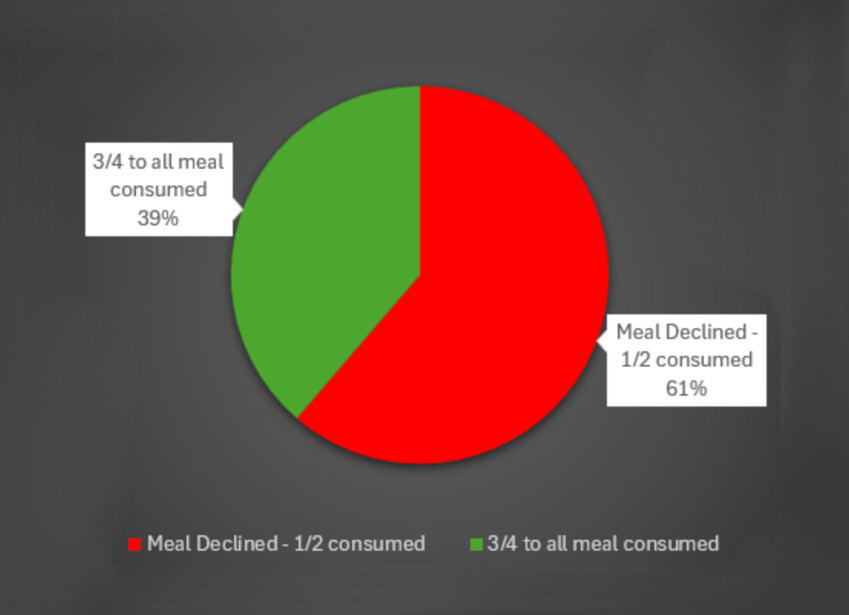
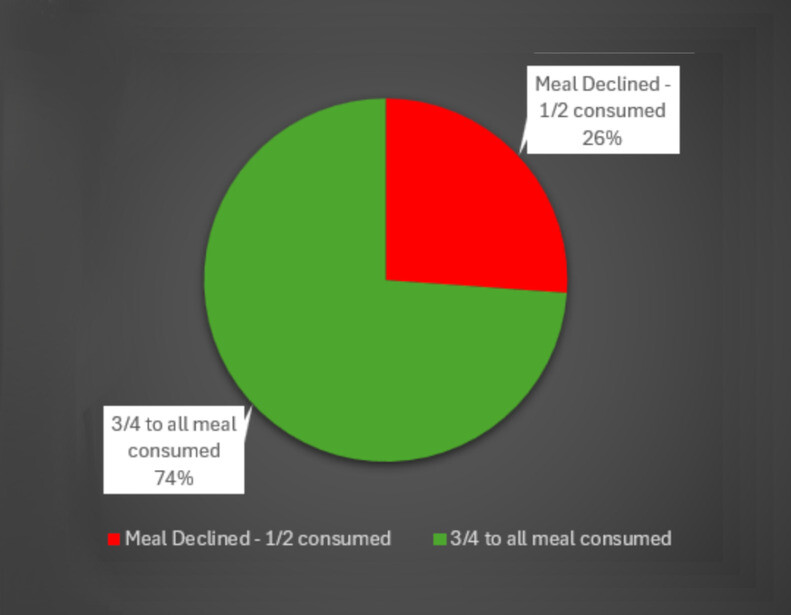
The first ward was at the EDGH, and staff were trained in small groups on the ward; all of whom were extremely positive about the D.I.E.T training they had been given and attended in groups of five so ward pressures were not affected. We collected data from each patients food charts to support our project prior to the staff being given the training. After they had the initial training we then collected a second set of data alongside a second questionnaire. To further support the evidence, Julie and Sharon collected a third set of data from food charts to ensure that the improvements were consistent.
The second ward was at Conquest Hospital, unfortunately the results from this ward were restricted due to a ward closure. However, despite this, positive results were still accumulated following the D.I.E.T training.
Conclusion
Overall, the D.I.E.T training was positively received, and there was a drastic change to the attitude and working practices of staff members following the training being given. Juie and Sharon have since attended a Dementia Steering Group, the Nutrition and Hydration Steering Group, an Urgent Care Governance Meeting, and the Quality Improvements Dragons Den, all of which found the outcome of the project staggering. The D.I.E.T training haws developed a very positive reputation within the hospital and Julie and Sharon are now being approached by by many staff members that are interested in undertaking the training themselves. The training will need to be monitored, this is due to the normality of attitudes prior to training being given, thus meaning that the staff must be held accountable to uphold all that they had learnt in the D.I.E.T training. They aim to follow the training up, and hold and hold staff accountable to the practices taught. It is hoped that this will result in all patients in hospital receiving a positive and enjoyable experience.
There is a noticeable improvement with food intake, however this will continue to be monitored as this will inform Julie and Sharon whether a bitesize training update will be required.